Prior Authorization & Eligibility
Approximately 16 hours per week or $80,000 per ordering physician per year. The delay is often over 30 days, impacting the ability to provide the best patient care.
Why so long? – Why so expensive? – Why so complex?
Get results with Empowered-Home.com:
Achievable Benefits

Reduced Cost of Labor
Reduce paid physician time from 16 hours per week down to minutes
Decrease the time providers spend on RFAI and requirements gathering

Improved Treatment Speed
Realtime adjudication allows immediate approval of the care plan
More accurate billing with fewer claim denials and faster reimbursement
Faster discharge and beds turnover

Customer Satisfaction
Better CSAT scores and patient referrals. Competitive advantage
Higher HVBP and HRRP rating for value-based programs
The Most Important Factors in Justification of a Prior Authorization Solution
Adoption of standards will accelerate automation and integration between payer/providers
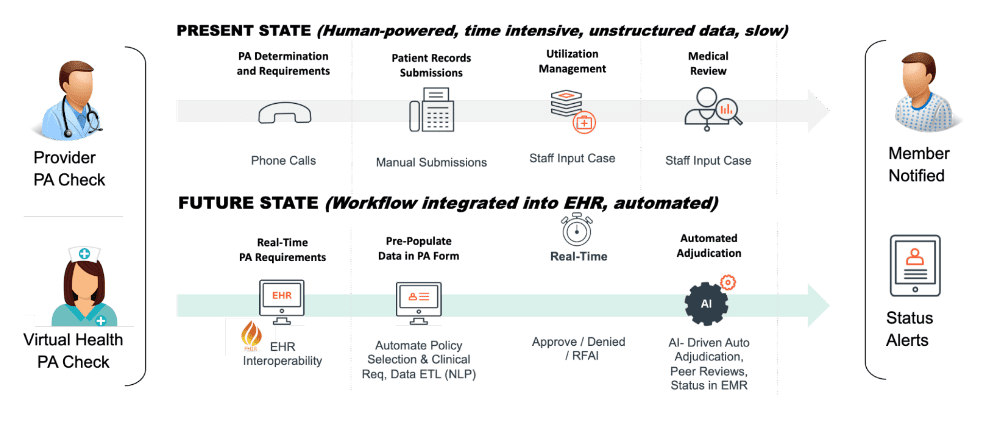
Improve patient outcomes: Get your patient orders approved faster. Reduce adverse events. Patients receive timely medically necessary care covered and reimbursed by payers.
Cost savings: Reduce Peer-to-Peer reviews and labor dollars spent on manual data entry. Improve the accuracy of requests and reduce the number of denied or delayed requests. Reduce costs tied to fewer hospitalizations and increase patient satisfaction and loyalty.
Improve efficiency: Automated prior authorization can streamline the PA process and reduce the need for manual work of Medical Assistants and staff. A policy support tool references standardized clinical guidelines to provide mutual trust between payers and clinicians.
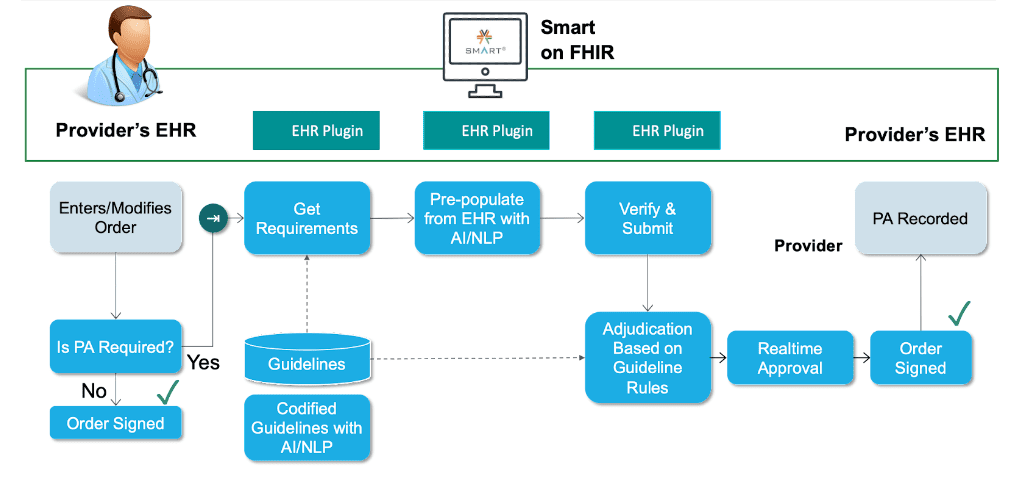
Reduce errors and denials: Automated prior authorization can help reduce errors using algorithms to verify information against codified medical necessity guidelines.
Patient Retention: Denials of prior authorization can contribute to patient leakage, particularly if the patient is unable to obtain the necessary treatment or procedure. In some cases, patients may switch physicians or payers in order to obtain timely treatment.
Improved data management: Automated prior authorization systems can help improve data management by capturing and storing data electronically, facilitating data analysis, and reporting tied to quality metrics and physician bonuses.
Regulatory compliance: Automated prior authorization systems can help ensure that physicians and payers are compliant with relevant regulations and policies.
Interested In Our Services?
Experience clinical and financial benefits with a quick turnaround.

